-
Reading Roadmap
- 1764-P: The Interplay between Pancreatic Mesenchymal Stem Cells and Macrophages in Obesity-Induced ß-Cell Dysfunction
- Key Takeaways
- Introduction: Unraveling the Complexities of Obesity-Induced ß-Cell Dysfunction
- The Role of PMSCs and Macrophages in ß-Cell Function
- Obesity Alters the Interaction between PMSCs and Macrophages
- Implications for Treatment of Obesity-Related Diabetes
- FAQ Section
- What are ß-cells?
- What are PMSCs and macrophages?
- How does obesity affect ß-cell function?
- How could understanding this interaction lead to new treatments for obesity-related diabetes?
- What further research is needed?
- Conclusion: The Future of Obesity-Related Diabetes Treatment
- Further Analysis
- Key Takeaways Revisited
1764-P: The Interplay between Pancreatic Mesenchymal Stem Cells and Macrophages in Obesity-Induced ß-Cell Dysfunction
[youtubomatic_search]
Key Takeaways
- Obesity can lead to ß-cell dysfunction, contributing to the development of type 2 diabetes.
- Pancreatic mesenchymal stem cells (PMSCs) and macrophages interact in the pancreas, influencing ß-cell function.
- Obesity alters the interaction between PMSCs and macrophages, promoting inflammation and ß-cell dysfunction.
- Understanding this interaction could lead to new therapeutic strategies for obesity-related diabetes.
- Further research is needed to fully understand the mechanisms involved in this interaction and its impact on ß-cell function.
Introduction: Unraveling the Complexities of Obesity-Induced ß-Cell Dysfunction
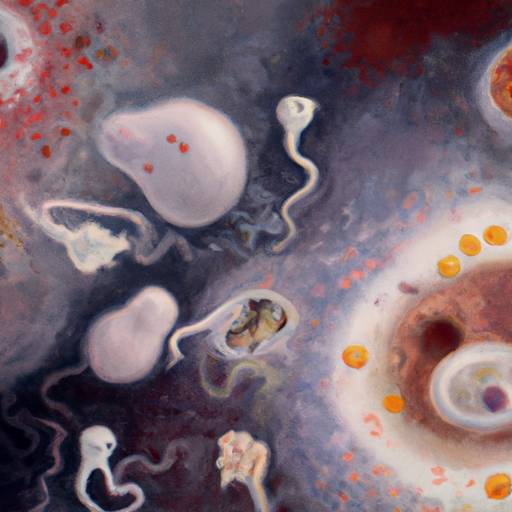
Obesity is a global health crisis, with a significant impact on the development of type 2 diabetes. A key factor in this process is ß-cell dysfunction, which impairs the body’s ability to regulate blood sugar levels. Recent research has shed light on the role of pancreatic mesenchymal stem cells (PMSCs) and macrophages in this process, revealing a complex interaction that is altered in obesity, leading to inflammation and ß-cell dysfunction.
The Role of PMSCs and Macrophages in ß-Cell Function
PMSCs are a type of stem cell found in the pancreas. They play a crucial role in maintaining the health and function of ß-cells, the cells responsible for producing insulin. Macrophages, a type of immune cell, also interact with PMSCs and ß-cells in the pancreas. Under normal conditions, this interaction helps to maintain ß-cell function and regulate immune responses in the pancreas.
Obesity Alters the Interaction between PMSCs and Macrophages
However, obesity changes the nature of this interaction. In obese individuals, PMSCs and macrophages promote inflammation in the pancreas. This inflammation impairs ß-cell function, leading to reduced insulin production and the development of type 2 diabetes. The exact mechanisms behind this altered interaction are still being investigated, but it is clear that it plays a significant role in obesity-induced ß-cell dysfunction.
Implications for Treatment of Obesity-Related Diabetes
Understanding the interaction between PMSCs and macrophages in obesity could lead to new therapeutic strategies for treating obesity-related diabetes. By targeting this interaction, it may be possible to reduce inflammation in the pancreas and restore ß-cell function, improving blood sugar regulation in obese individuals. However, further research is needed to fully understand the mechanisms involved and to develop effective treatments.
FAQ Section
What are ß-cells?
ß-cells are a type of cell in the pancreas that produce insulin, a hormone that regulates blood sugar levels.
What are PMSCs and macrophages?
PMSCs are a type of stem cell found in the pancreas, while macrophages are a type of immune cell. Both interact with ß-cells in the pancreas and play a role in maintaining their function.
How does obesity affect ß-cell function?
Obesity alters the interaction between PMSCs and macrophages in the pancreas, promoting inflammation and impairing ß-cell function. This leads to reduced insulin production and the development of type 2 diabetes.
How could understanding this interaction lead to new treatments for obesity-related diabetes?
By targeting the interaction between PMSCs and macrophages, it may be possible to reduce inflammation in the pancreas and restore ß-cell function, improving blood sugar regulation in obese individuals.
What further research is needed?
Further research is needed to fully understand the mechanisms involved in the interaction between PMSCs and macrophages in obesity and its impact on ß-cell function. This will help to develop effective treatments for obesity-related diabetes.
Conclusion: The Future of Obesity-Related Diabetes Treatment
The interaction between PMSCs and macrophages in the pancreas plays a crucial role in ß-cell function, and this interaction is altered in obesity, leading to inflammation and ß-cell dysfunction. Understanding this interaction could open up new avenues for the treatment of obesity-related diabetes, offering hope for the millions of people worldwide affected by this condition. However, further research is needed to fully understand the mechanisms involved and to develop effective treatments.
[youtubomatic_search]
Further Analysis
As we delve deeper into the complexities of obesity-induced ß-cell dysfunction, it becomes clear that the interaction between PMSCs and macrophages is a key piece of the puzzle. By continuing to investigate this interaction and its impact on ß-cell function, we can move closer to developing effective treatments for obesity-related diabetes, a condition that affects millions of people worldwide.
Key Takeaways Revisited
- Obesity can lead to ß-cell dysfunction, contributing to the development of type 2 diabetes.
- Pancreatic mesenchymal stem cells (PMSCs) and macrophages interact in the pancreas, influencing ß-cell function.
- Obesity alters the interaction between PMSCs and macrophages, promoting inflammation and ß-cell dysfunction.
- Understanding this interaction could lead to new therapeutic strategies for obesity-related diabetes.
- Further research is needed to fully understand the mechanisms involved in this interaction and its impact on ß-cell function.

Leave a Reply