-
Reading Roadmap
- 113-OR: The Role of Lipocalin-2 as a Mitokine in Facilitating Communication Between White and Brown Fat Cells
- Key Takeaways
- Introduction: Unraveling the Role of Lipocalin-2
- The Function of Lipocalin-2
- Lipocalin-2 as a Satiety Factor
- Implications for Obesity and Metabolic Disorders
- Future Directions
- FAQ Section
- Conclusion: The Potential of Lipocalin-2
- Further Analysis
- Key Takeaways Revisited
113-OR: The Role of Lipocalin-2 as a Mitokine in Facilitating Communication Between White and Brown Fat Cells
[youtubomatic_search]
Key Takeaways
- Lipocalin-2 (LCN2) is a mitokine that plays a crucial role in facilitating communication between white and brown fat cells.
- LCN2 is secreted by muscles during exercise and can stimulate the browning of white fat cells, leading to increased energy expenditure and improved metabolic health.
- Recent studies have shown that LCN2 can also act as a satiety factor, reducing food intake and promoting weight loss.
- Understanding the role of LCN2 in fat cell communication could lead to new therapeutic strategies for obesity and related metabolic disorders.
- Further research is needed to fully understand the mechanisms through which LCN2 exerts its effects and to explore its potential as a therapeutic target.
Introduction: Unraveling the Role of Lipocalin-2
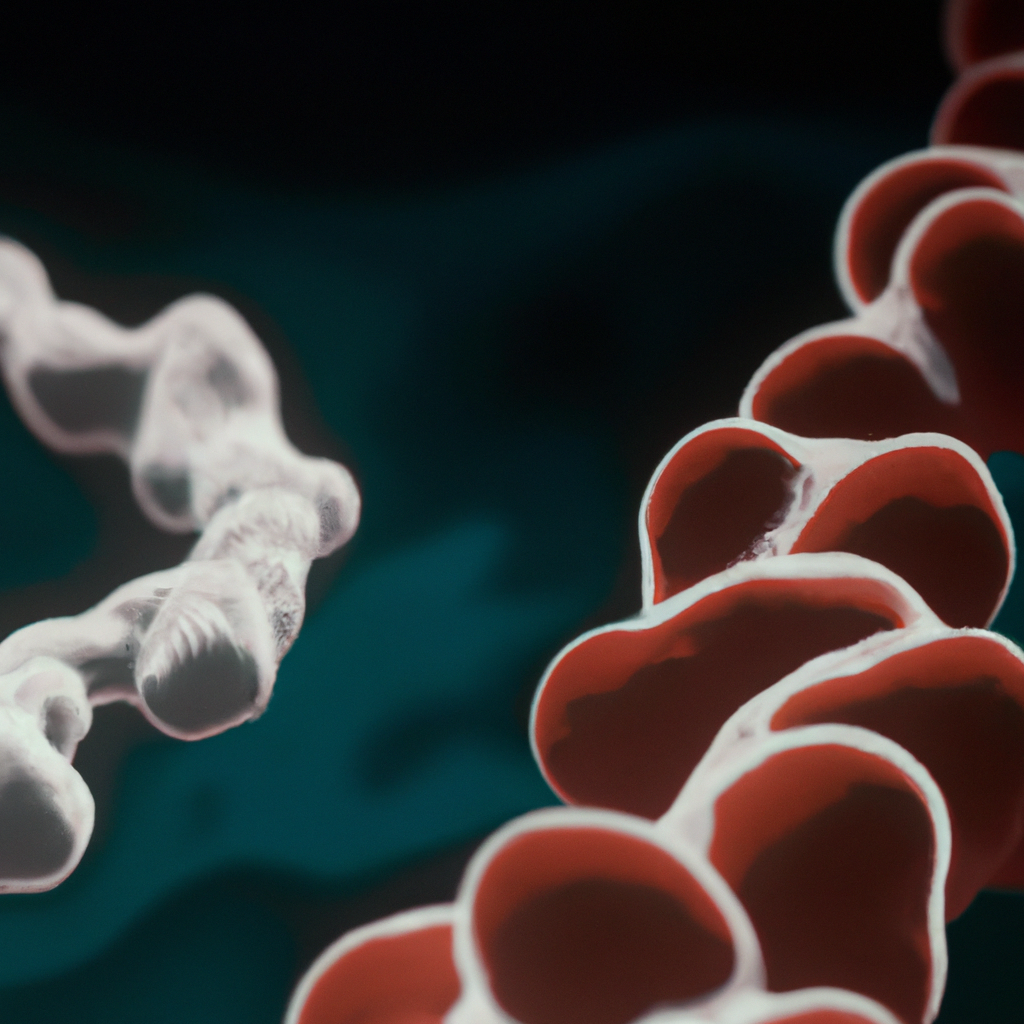
The growing prevalence of obesity and related metabolic disorders has spurred intense research into the mechanisms that regulate energy balance and fat storage. One area of focus is the communication between different types of fat cells, particularly white and brown adipocytes. This article delves into the role of Lipocalin-2 (LCN2), a mitokine secreted by muscles during exercise, in facilitating this intercellular communication and its implications for metabolic health.
The Function of Lipocalin-2
LCN2 is a protein that is secreted by muscles during exercise and has been found to stimulate the browning of white fat cells. This process, known as “browning,” involves the conversion of white fat cells, which store energy, into brown fat cells, which burn energy to produce heat. By promoting this conversion, LCN2 can increase energy expenditure and improve metabolic health.
Lipocalin-2 as a Satiety Factor
Recent studies have also revealed a new role for LCN2 as a satiety factor. Researchers found that LCN2 can bind to receptors in the hypothalamus, a region of the brain that regulates appetite, and signal satiety, thereby reducing food intake. This discovery suggests that LCN2 could potentially be used as a therapeutic agent to promote weight loss.
Implications for Obesity and Metabolic Disorders
The ability of LCN2 to stimulate the browning of white fat cells and reduce food intake makes it a promising target for the treatment of obesity and related metabolic disorders. By enhancing the body’s natural energy-burning capabilities and reducing overeating, LCN2 could help to restore energy balance and improve metabolic health.
Future Directions
Despite these promising findings, much remains to be understood about the role of LCN2 in fat cell communication and metabolic regulation. Further research is needed to elucidate the mechanisms through which LCN2 exerts its effects and to explore its potential as a therapeutic target.
FAQ Section
- What is Lipocalin-2? Lipocalin-2 (LCN2) is a protein that is secreted by muscles during exercise. It plays a crucial role in facilitating communication between white and brown fat cells.
- What is the role of LCN2 in fat cell communication? LCN2 stimulates the browning of white fat cells, leading to increased energy expenditure. It can also act as a satiety factor, reducing food intake.
- How can LCN2 improve metabolic health? By promoting the conversion of white fat cells into energy-burning brown fat cells and reducing overeating, LCN2 can help to restore energy balance and improve metabolic health.
- Can LCN2 be used as a therapeutic agent? The ability of LCN2 to stimulate the browning of white fat cells and reduce food intake makes it a promising target for the treatment of obesity and related metabolic disorders.
- What further research is needed? Further research is needed to fully understand the mechanisms through which LCN2 exerts its effects and to explore its potential as a therapeutic target.
Conclusion: The Potential of Lipocalin-2
The role of Lipocalin-2 in facilitating communication between white and brown fat cells offers exciting possibilities for the treatment of obesity and related metabolic disorders. By promoting the browning of white fat cells and acting as a satiety factor, LCN2 could help to restore energy balance and improve metabolic health. However, further research is needed to fully understand the mechanisms through which LCN2 exerts its effects and to explore its potential as a therapeutic target.
[youtubomatic_search]
Further Analysis
As we delve deeper into the role of Lipocalin-2, it becomes clear that this mitokine holds significant potential in the fight against obesity and metabolic disorders. Its ability to facilitate communication between white and brown fat cells, stimulate the browning of white fat cells, and act as a satiety factor positions it as a promising therapeutic target. However, the journey to fully understand and harness the potential of LCN2 is just beginning, and further research is crucial.
Key Takeaways Revisited
- Lipocalin-2 plays a crucial role in facilitating communication between white and brown fat cells.
- It is secreted by muscles during exercise and can stimulate the browning of white fat cells, leading to increased energy expenditure.
- LCN2 can also act as a satiety factor, reducing food intake and promoting weight loss.
- Understanding the role of LCN2 could lead to new therapeutic strategies for obesity and related metabolic disorders.
- Further research is needed to fully understand the mechanisms through which LCN2 exerts its effects and to explore its potential as a therapeutic target.