-
Reading Roadmap
- 859-P: Successful Targeting of Hepatic Ketohexokinase by ALN-KHK, an Experimental RNA Interference Therapeutic, in a Single Ascending Dose Study on Overweight to Obese Adults
- Key Takeaways
- Introduction: A New Frontier in Metabolic Disorder Treatment
- RNA Interference: A Revolutionary Technique
- ALN-KHK: A Potential Game-Changer
- Further Research Needed
- FAQ Section
- What is ALN-KHK?
- What is RNA interference?
- What diseases could ALN-KHK potentially treat?
- What were the results of the single ascending dose study of ALN-KHK?
- What further research is needed?
- Conclusion: A Promising Step Forward
- Key Takeaways Revisited
859-P: Successful Targeting of Hepatic Ketohexokinase by ALN-KHK, an Experimental RNA Interference Therapeutic, in a Single Ascending Dose Study on Overweight to Obese Adults
[youtubomatic_search]
Key Takeaways
- ALN-KHK, an experimental RNA interference therapeutic, has shown promising results in targeting hepatic ketohexokinase in a single ascending dose study on overweight to obese adults.
- The study indicates that ALN-KHK could potentially be a novel treatment for metabolic disorders, including non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes.
- RNA interference (RNAi) is a revolutionary technique that allows for the silencing of specific genes, potentially leading to new treatments for a variety of diseases.
- The study demonstrated a significant reduction in fructose-induced lipogenesis, a key factor in the development of NAFLD and type 2 diabetes.
- Further research is needed to confirm these findings and to determine the long-term safety and efficacy of ALN-KHK.
Introduction: A New Frontier in Metabolic Disorder Treatment
Metabolic disorders, including non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes, are a growing global health concern. Traditional treatments have often fallen short, leading researchers to explore novel therapeutic approaches. One such approach is the use of RNA interference (RNAi) therapeutics, such as ALN-KHK, which target specific genes involved in disease development. This article delves into the promising results of a single ascending dose study of ALN-KHK on overweight to obese adults.
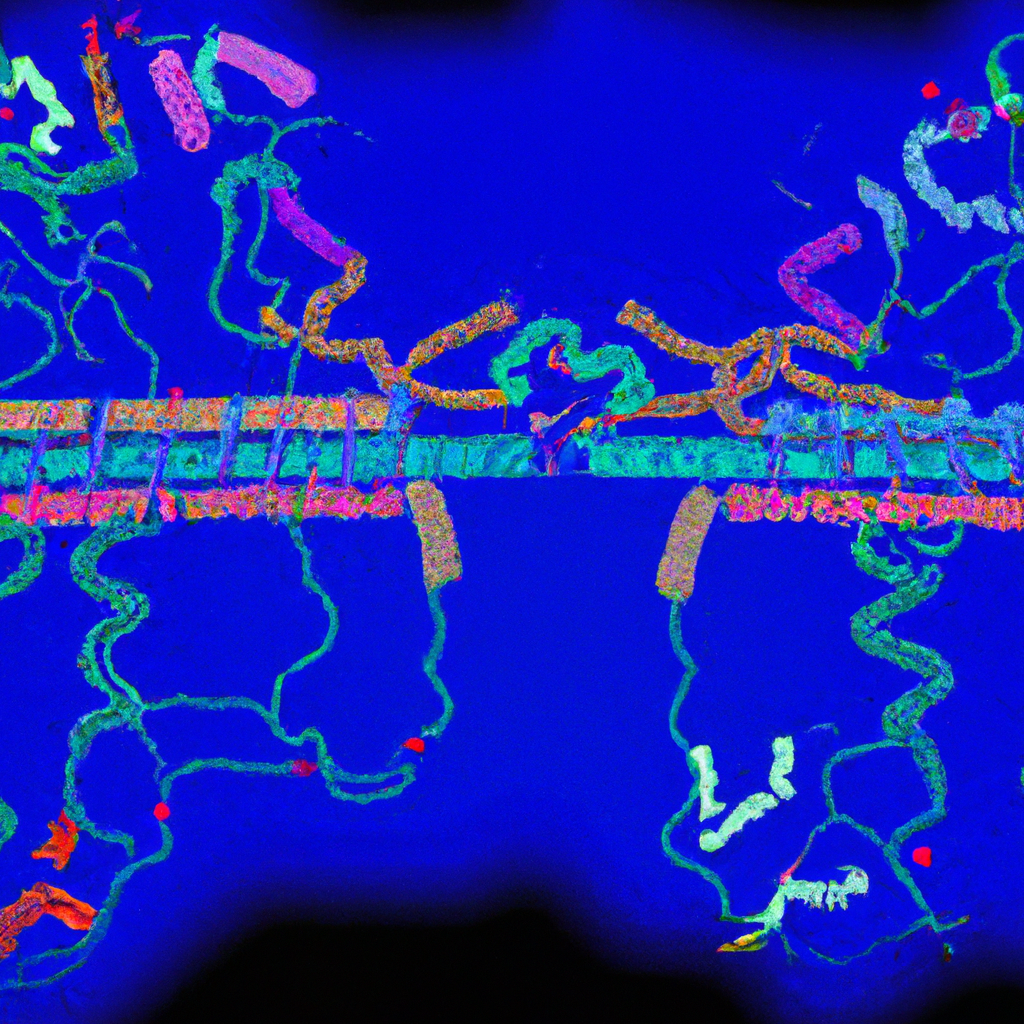
RNA Interference: A Revolutionary Technique
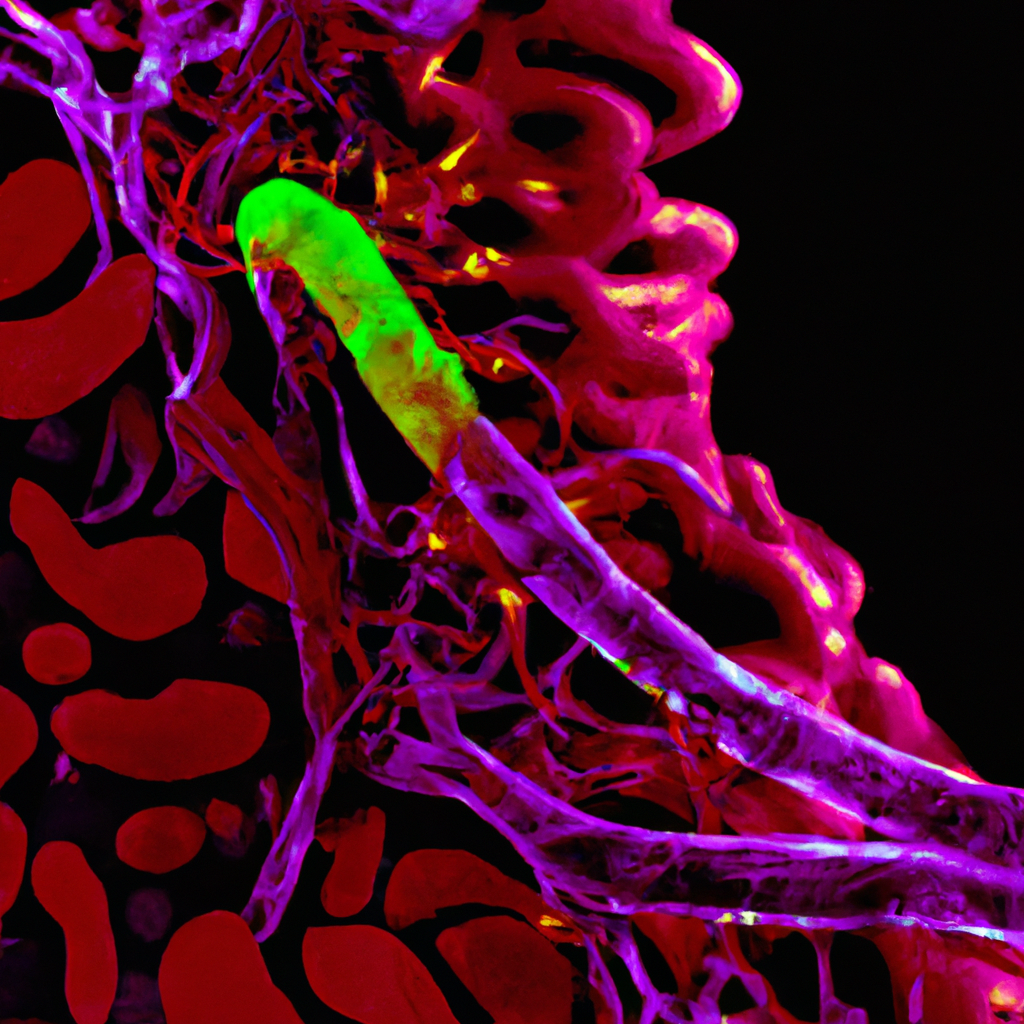
RNA interference (RNAi) is a biological process in which RNA molecules inhibit gene expression, effectively “silencing” specific genes. This technique has the potential to revolutionize the treatment of a variety of diseases, including metabolic disorders. ALN-KHK, an experimental RNAi therapeutic, targets the hepatic ketohexokinase (KHK) gene, which plays a crucial role in fructose metabolism and is implicated in the development of NAFLD and type 2 diabetes.
ALN-KHK: A Potential Game-Changer
The single ascending dose study of ALN-KHK on overweight to obese adults demonstrated promising results. The study showed that ALN-KHK significantly reduced fructose-induced lipogenesis, a key factor in the development of NAFLD and type 2 diabetes. This suggests that ALN-KHK could potentially be a novel treatment for these metabolic disorders.
Further Research Needed
While the results of the study are promising, further research is needed to confirm these findings and to determine the long-term safety and efficacy of ALN-KHK. Future studies should also explore the potential of ALN-KHK in treating other diseases associated with the KHK gene.
[youtubomatic_search]
FAQ Section
What is ALN-KHK?
ALN-KHK is an experimental RNA interference (RNAi) therapeutic that targets the hepatic ketohexokinase (KHK) gene.
What is RNA interference?
RNA interference (RNAi) is a biological process in which RNA molecules inhibit gene expression, effectively “silencing” specific genes.
What diseases could ALN-KHK potentially treat?
ALN-KHK could potentially treat metabolic disorders, including non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes.
What were the results of the single ascending dose study of ALN-KHK?
The study showed that ALN-KHK significantly reduced fructose-induced lipogenesis, a key factor in the development of NAFLD and type 2 diabetes.
What further research is needed?
Further research is needed to confirm these findings and to determine the long-term safety and efficacy of ALN-KHK. Future studies should also explore the potential of ALN-KHK in treating other diseases associated with the KHK gene.
Conclusion: A Promising Step Forward
The single ascending dose study of ALN-KHK on overweight to obese adults represents a promising step forward in the treatment of metabolic disorders. By successfully targeting the hepatic ketohexokinase gene, ALN-KHK has the potential to revolutionize the treatment of diseases such as NAFLD and type 2 diabetes. However, further research is needed to confirm these findings and to determine the long-term safety and efficacy of this experimental RNAi therapeutic.
Key Takeaways Revisited
- ALN-KHK, an experimental RNA interference therapeutic, has shown promising results in targeting hepatic ketohexokinase in a single ascending dose study on overweight to obese adults.
- The study indicates that ALN-KHK could potentially be a novel treatment for metabolic disorders, including non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes.
- RNA interference (RNAi) is a revolutionary technique that allows for the silencing of specific genes, potentially leading to new treatments for a variety of diseases.
- The study demonstrated a significant reduction in fructose-induced lipogenesis, a key factor in the development of NAFLD and type 2 diabetes.
- Further research is needed to confirm these findings and to determine the long-term safety and efficacy of ALN-KHK.