-
Reading Roadmap
- Promoting Diabetes Self-Management through Personalized Digital Experiences: A Mixed Methods Social Computing Approach
- Key Takeaways
- Introduction: The Digital Revolution in Diabetes Management
- The Power of Personalized Digital Experiences
- Social Computing: A Platform for Peer Support and Shared Learning
- Technology for Tracking and Analyzing Health Data
- Healthcare Providers and Digital Platforms
- FAQ Section
- 1. How can personalized digital experiences enhance diabetes self-management?
- 2. How can social computing approaches support individuals with diabetes?
- 3. How can technology help in tracking and analyzing health data?
- 4. How can healthcare providers use digital platforms?
- 5. What are the challenges in using digital technology for diabetes management?
- Conclusion: The Future of Diabetes Management
- Further Analysis
- Key Takeaways Revisited
Promoting Diabetes Self-Management through Personalized Digital Experiences: A Mixed Methods Social Computing Approach

[youtubomatic_search]
Key Takeaways
- Personalized digital experiences can significantly enhance diabetes self-management.
- Social computing approaches can provide a platform for peer support and shared learning.
- Technology can help in tracking and analyzing health data, leading to better health outcomes.
- Healthcare providers can use digital platforms to monitor patients’ progress and provide timely interventions.
- Despite the potential benefits, there are challenges in terms of privacy, data security, and digital literacy that need to be addressed.
Introduction: The Digital Revolution in Diabetes Management
Diabetes is a chronic condition that requires continuous self-management. With the advent of digital technology, there has been a paradigm shift in the way diabetes care is delivered. This article explores how personalized digital experiences, underpinned by a mixed methods social computing approach, can promote diabetes self-management.
The Power of Personalized Digital Experiences
Personalized digital experiences can empower individuals with diabetes to take control of their health. For instance, mobile apps can provide personalized diet and exercise plans, reminders for medication, and real-time feedback on blood glucose levels. A study by Quinn et al. (2011) found that a mobile diabetes management system improved glycemic control in adults with type 2 diabetes.
Social Computing: A Platform for Peer Support and Shared Learning
Social computing approaches, such as online communities and social media platforms, can provide a platform for peer support and shared learning. According to a study by Litchman et al. (2018), online diabetes communities can provide emotional support, practical advice, and a sense of belonging. Moreover, they can facilitate shared learning, where individuals learn from each other’s experiences and insights.
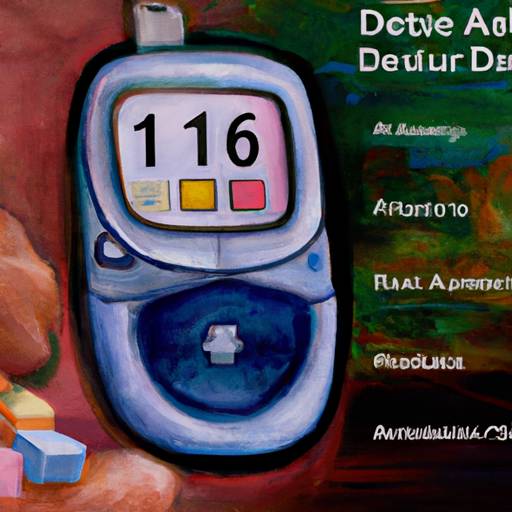
Technology for Tracking and Analyzing Health Data
Technology can help in tracking and analyzing health data, leading to better health outcomes. For example, wearable devices can continuously monitor blood glucose levels, providing valuable data for managing diabetes. Furthermore, artificial intelligence can analyze this data to predict blood glucose trends and provide personalized recommendations. A study by Contreras et al. (2019) found that a machine learning model could predict blood glucose levels with high accuracy.
Healthcare Providers and Digital Platforms
Healthcare providers can use digital platforms to monitor patients’ progress and provide timely interventions. For instance, telemedicine can enable remote consultations, reducing the need for physical visits. Moreover, healthcare providers can use data from digital platforms to identify patients at risk and provide targeted interventions. A study by Greenwood et al. (2017) found that a digital diabetes management program led to significant improvements in glycemic control.
FAQ Section
1. How can personalized digital experiences enhance diabetes self-management?
Personalized digital experiences, such as mobile apps, can provide personalized diet and exercise plans, reminders for medication, and real-time feedback on blood glucose levels, thereby enhancing diabetes self-management.
2. How can social computing approaches support individuals with diabetes?
Social computing approaches, such as online communities and social media platforms, can provide a platform for peer support and shared learning, thereby supporting individuals with diabetes.
3. How can technology help in tracking and analyzing health data?
Technology, such as wearable devices and artificial intelligence, can help in tracking and analyzing health data, thereby leading to better health outcomes.
4. How can healthcare providers use digital platforms?
Healthcare providers can use digital platforms to monitor patients’ progress and provide timely interventions, thereby improving diabetes care.
5. What are the challenges in using digital technology for diabetes management?
Despite the potential benefits, there are challenges in terms of privacy, data security, and digital literacy that need to be addressed.
Conclusion: The Future of Diabetes Management
Personalized digital experiences, underpinned by a mixed methods social computing approach, can significantly enhance diabetes self-management. They can empower individuals with diabetes to take control of their health, provide a platform for peer support and shared learning, and help in tracking and analyzing health data. Moreover, healthcare providers can use digital platforms to monitor patients’ progress and provide timely interventions. However, there are challenges that need to be addressed, including privacy, data security, and digital literacy. As we move forward, it is crucial to harness the power of digital technology while addressing these challenges, to transform diabetes care.
[youtubomatic_search]
Further Analysis
As we delve deeper into the digital revolution in diabetes management, it is clear that personalized digital experiences and social computing approaches hold great promise. However, it is equally important to address the challenges and ensure that digital technology is accessible, secure, and user-friendly. Future research should focus on developing innovative solutions, evaluating their effectiveness, and exploring ways to overcome the barriers. With the right approach, digital technology can truly revolutionize diabetes care.
Key Takeaways Revisited
- Personalized digital experiences can significantly enhance diabetes self-management.
- Social computing approaches can provide a platform for peer support and shared learning.
- Technology can help in tracking and analyzing health data, leading to better health outcomes.
- Healthcare providers can use digital platforms to monitor patients’ progress and provide timely interventions.
- Despite the potential benefits, there are challenges in terms of privacy, data security, and digital literacy that need to be addressed.