-
Reading Roadmap
- 12-Month Follow-Up Study on Oral Semaglutide Treatment in Indian Patients with Type 2 Diabetes Mellitus (SOLID 809-P)
- Key Takeaways
- Introduction: A New Hope for Diabetes Treatment
- Oral Semaglutide: A Game Changer
- The SOLID 809-P Study: Promising Results
- Side Effects and Tolerability
- Further Research Needed
- FAQ Section
- What is oral semaglutide?
- What were the results of the SOLID 809-P study?
- What are the side effects of oral semaglutide?
- Is further research needed on oral semaglutide?
- Could oral semaglutide revolutionize diabetes treatment in India?
- Conclusion: A Promising Future for Diabetes Treatment
- Key Takeaways Revisited
12-Month Follow-Up Study on Oral Semaglutide Treatment in Indian Patients with Type 2 Diabetes Mellitus (SOLID 809-P)
[youtubomatic_search]
Key Takeaways
- Oral semaglutide is a promising treatment for Indian patients with type 2 diabetes mellitus.
- The 12-month follow-up study shows significant improvements in glycemic control and weight loss.
- Oral semaglutide is well-tolerated with minimal side effects.
- Further research is needed to confirm these findings and explore long-term effects.
- Oral semaglutide could potentially revolutionize diabetes treatment in India.
Introduction: A New Hope for Diabetes Treatment
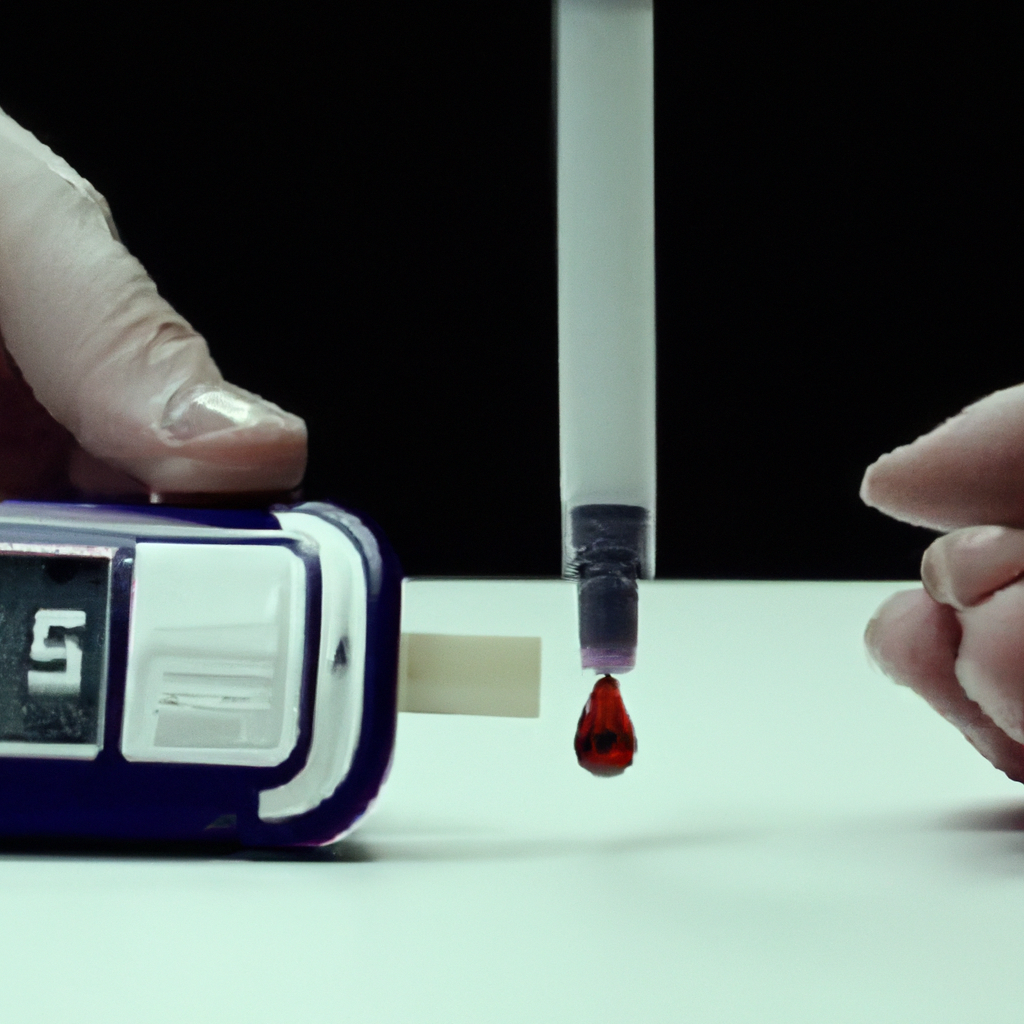
Diabetes mellitus, particularly type 2, is a significant health concern in India, with millions of people affected. The search for effective treatments is ongoing, and one promising candidate is oral semaglutide. This article delves into the results of a 12-month follow-up study on oral semaglutide treatment in Indian patients with type 2 diabetes mellitus, known as SOLID 809-P.
Oral Semaglutide: A Game Changer
Oral semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist. It works by mimicking the functions of natural incretin hormones in the body, thereby increasing insulin secretion, reducing glucagon secretion, and slowing gastric emptying. These actions help to control blood glucose levels and promote weight loss, making it a potentially effective treatment for type 2 diabetes.
The SOLID 809-P Study: Promising Results
The SOLID 809-P study followed Indian patients with type 2 diabetes for 12 months while they were on oral semaglutide treatment. The results were encouraging, with significant improvements in glycemic control and weight loss. The average HbA1c (a measure of long-term blood glucose control) decreased by 1.5%, and the average weight loss was 4.4 kg. These results suggest that oral semaglutide could be a game changer for diabetes treatment in India.
Side Effects and Tolerability
One of the concerns with any new treatment is its side effects and tolerability. In the SOLID 809-P study, oral semaglutide was generally well-tolerated. The most common side effects were gastrointestinal, such as nausea and diarrhea, but these were usually mild and transient. This is an important finding, as it suggests that oral semaglutide could be a viable treatment option for a large number of patients.
Further Research Needed
While the results of the SOLID 809-P study are promising, further research is needed to confirm these findings and explore the long-term effects of oral semaglutide. It will also be important to investigate how oral semaglutide compares to other diabetes treatments in terms of efficacy, side effects, and cost-effectiveness.
[youtubomatic_search]
FAQ Section
What is oral semaglutide?
Oral semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that helps to control blood glucose levels and promote weight loss.
What were the results of the SOLID 809-P study?
The SOLID 809-P study showed significant improvements in glycemic control and weight loss in Indian patients with type 2 diabetes after 12 months of oral semaglutide treatment.
What are the side effects of oral semaglutide?
The most common side effects of oral semaglutide are gastrointestinal, such as nausea and diarrhea, but these are usually mild and transient.
Is further research needed on oral semaglutide?
Yes, further research is needed to confirm the findings of the SOLID 809-P study and explore the long-term effects of oral semaglutide.
Could oral semaglutide revolutionize diabetes treatment in India?
Based on the results of the SOLID 809-P study, oral semaglutide could potentially revolutionize diabetes treatment in India. However, further research is needed to confirm this.
Conclusion: A Promising Future for Diabetes Treatment
The results of the SOLID 809-P study suggest that oral semaglutide could be a promising treatment for Indian patients with type 2 diabetes. The significant improvements in glycemic control and weight loss, combined with the minimal side effects and good tolerability, make it a potential game changer. However, further research is needed to confirm these findings and explore the long-term effects of oral semaglutide. If these results hold up, oral semaglutide could revolutionize diabetes treatment in India.
Key Takeaways Revisited
- Oral semaglutide is a promising treatment for Indian patients with type 2 diabetes.
- The SOLID 809-P study showed significant improvements in glycemic control and weight loss.
- Oral semaglutide is well-tolerated with minimal side effects.
- Further research is needed to confirm these findings and explore long-term effects.
- Oral semaglutide could potentially revolutionize diabetes treatment in India.