-
Reading Roadmap
- Effective Integration of Stem Cell-Derived Islets into Vascular and Neural Systems
- Key Takeaways
- Introduction: The Promise of Stem Cell-Derived Islets
- Understanding the Integration Process
- Challenges and Potential Solutions
- FAQ Section
- What are stem cell-derived islets?
- Why is the integration of these islets important?
- What are the main challenges in the integration process?
- What are some potential solutions to these challenges?
- What is the potential impact of successful integration?
- Conclusion: The Future of Stem Cell-Derived Islets
- Further Analysis
- Key Takeaways Revisited
Effective Integration of Stem Cell-Derived Islets into Vascular and Neural Systems
[youtubomatic_search]
Key Takeaways
- Stem cell-derived islets have the potential to revolutionize treatment for diabetes and other diseases.
- Successful integration of these islets into vascular and neural systems is crucial for their functionality.
- Recent research has made significant strides in improving the integration process.
- Challenges remain, including the need for more effective methods of vascularization and innervation.
- Continued research and development in this field could lead to breakthroughs in regenerative medicine.
Introduction: The Promise of Stem Cell-Derived Islets
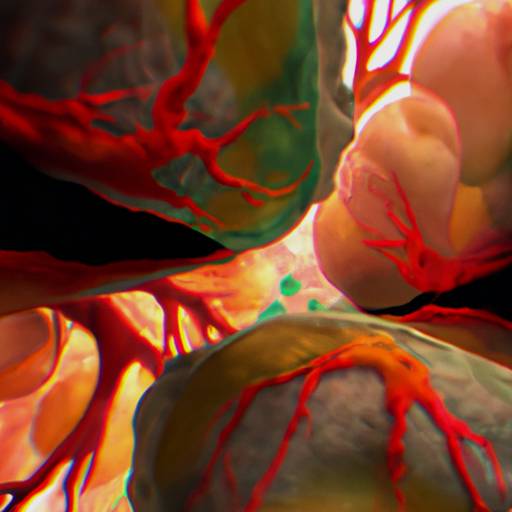
Stem cell-derived islets, also known as islet-like clusters (ILCs), hold immense promise for the treatment of diseases such as diabetes. These clusters of cells, derived from pluripotent stem cells, have the potential to replace damaged or non-functioning islets in the pancreas, thereby restoring the body’s ability to regulate blood sugar levels. However, for these ILCs to function effectively, they must be successfully integrated into the body’s vascular and neural systems. This article explores the current state of research in this field, the challenges faced, and the potential solutions on the horizon.
Understanding the Integration Process
The integration of stem cell-derived islets into the body’s systems is a complex process. It involves not only the transplantation of the islets themselves, but also their vascularization (the formation of new blood vessels) and innervation (the supply of nerves). Both of these processes are crucial for the islets to receive the necessary nutrients and signals to function effectively.
Recent research has made significant strides in improving the integration process. For example, a study published in the journal “Cell Reports” demonstrated that the use of a bioengineered scaffold could enhance the vascularization of transplanted islets, improving their survival and function. Another study, published in “Nature Biotechnology”, showed that the use of a hydrogel could improve the innervation of transplanted islets, enhancing their ability to regulate blood sugar levels.
Challenges and Potential Solutions
Despite these advances, challenges remain in the integration of stem cell-derived islets. One of the main challenges is the need for more effective methods of vascularization and innervation. Current methods often result in the formation of blood vessels and nerves that are not fully functional, limiting the effectiveness of the transplanted islets.
Research is ongoing to develop more effective methods. For example, a team of researchers at the University of California, San Francisco, is exploring the use of bioengineered blood vessels to improve the vascularization of transplanted islets. Another team at the University of Toronto is investigating the use of nerve growth factors to enhance the innervation of transplanted islets.
FAQ Section
What are stem cell-derived islets?
Stem cell-derived islets, or islet-like clusters, are clusters of cells derived from pluripotent stem cells. They have the potential to replace damaged or non-functioning islets in the pancreas, which are crucial for regulating blood sugar levels.
Why is the integration of these islets important?
For stem cell-derived islets to function effectively, they must be successfully integrated into the body’s vascular and neural systems. This allows them to receive the necessary nutrients and signals to function effectively.
What are the main challenges in the integration process?
The main challenges in the integration process are the need for more effective methods of vascularization and innervation. Current methods often result in the formation of blood vessels and nerves that are not fully functional, limiting the effectiveness of the transplanted islets.
What are some potential solutions to these challenges?
Research is ongoing to develop more effective methods of vascularization and innervation. This includes the use of bioengineered blood vessels and nerve growth factors.
What is the potential impact of successful integration?
Successful integration of stem cell-derived islets could revolutionize the treatment of diseases such as diabetes, leading to breakthroughs in regenerative medicine.
Conclusion: The Future of Stem Cell-Derived Islets
The integration of stem cell-derived islets into vascular and neural systems is a complex but crucial process. While challenges remain, recent research has made significant strides in improving the integration process. With continued research and development, the successful integration of these islets could revolutionize the treatment of diseases such as diabetes, leading to breakthroughs in regenerative medicine.
[youtubomatic_search]
Further Analysis
As we continue to explore the potential of stem cell-derived islets, it is clear that the key to their success lies in their effective integration into the body’s systems. With ongoing research and development, we can look forward to a future where diseases like diabetes can be treated more effectively and potentially even cured.
Key Takeaways Revisited
- Stem cell-derived islets hold immense promise for the treatment of diseases such as diabetes.
- Successful integration into the body’s vascular and neural systems is crucial for their functionality.
- Recent research has made significant strides in improving the integration process.
- Challenges remain, including the need for more effective methods of vascularization and innervation.
- Continued research and development could lead to breakthroughs in regenerative medicine.

Leave a Reply