-
Reading Roadmap
- SARS-CoV-2 Spike S1 Subunit Induces Dysfunction in Pericyte and Microvascular of Human Pancreatic Islets
- Key Takeaways
- Introduction: Unraveling the Impact of SARS-CoV-2 on the Pancreas
- The SARS-CoV-2 Spike S1 Subunit and the Pancreas
- Implications for COVID-19 Patients
- Future Research and Potential Treatments
- FAQ Section
- What is the SARS-CoV-2 spike S1 subunit?
- How does the S1 subunit cause dysfunction in the pancreas?
- What are the implications of this dysfunction for COVID-19 patients?
- What further research is needed?
- Could this research lead to new treatments for COVID-19 related diabetes?
- Conclusion: The Crucial Role of the SARS-CoV-2 Spike S1 Subunit in Pancreatic Dysfunction
- Key Takeaways Revisited
SARS-CoV-2 Spike S1 Subunit Induces Dysfunction in Pericyte and Microvascular of Human Pancreatic Islets
[youtubomatic_search]
Key Takeaways
- The SARS-CoV-2 spike S1 subunit can cause dysfunction in the pericyte and microvascular of human pancreatic islets.
- This dysfunction can lead to diabetes-like symptoms in COVID-19 patients.
- Research indicates that the S1 subunit can bind to ACE2 receptors in the pancreas, causing inflammation and cell death.
- Further studies are needed to fully understand the long-term effects of this interaction.
- Understanding this mechanism could lead to new treatments for COVID-19 related diabetes.
Introduction: Unraveling the Impact of SARS-CoV-2 on the Pancreas
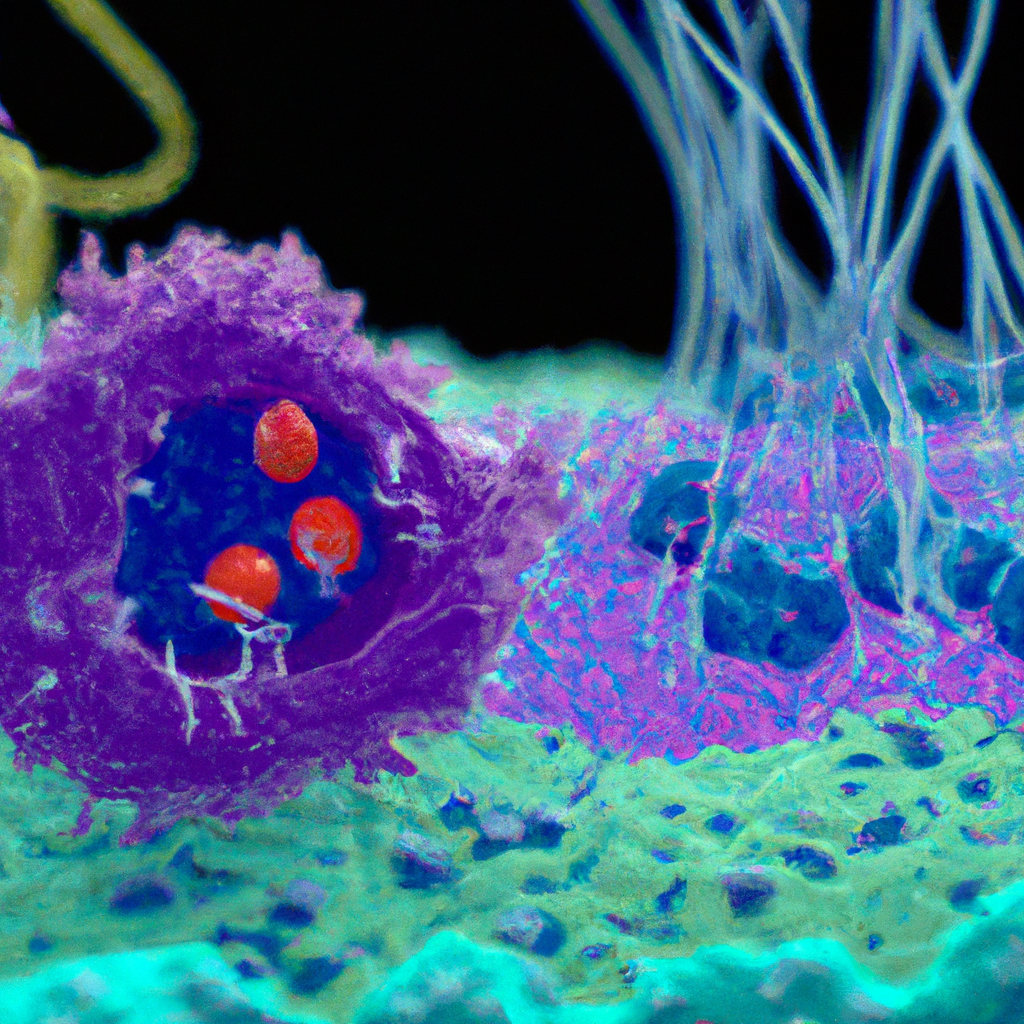
Since the outbreak of the COVID-19 pandemic, caused by the SARS-CoV-2 virus, scientists have been working tirelessly to understand the virus’s effects on the human body. One area of particular interest is the virus’s impact on the pancreas, specifically the pericyte and microvascular of human pancreatic islets. Recent research suggests that the SARS-CoV-2 spike S1 subunit can cause significant dysfunction in these areas, potentially leading to diabetes-like symptoms in COVID-19 patients.
The SARS-CoV-2 Spike S1 Subunit and the Pancreas
The SARS-CoV-2 virus uses its spike S1 subunit to bind to ACE2 receptors on human cells, allowing it to enter and infect the cell. These ACE2 receptors are found in many parts of the body, including the pancreas. When the S1 subunit binds to these receptors in the pancreas, it can cause inflammation and cell death, leading to dysfunction in the pericyte and microvascular of human pancreatic islets.
Implications for COVID-19 Patients
This dysfunction can have serious implications for COVID-19 patients. The pericyte and microvascular of human pancreatic islets play a crucial role in regulating blood sugar levels. When these areas are damaged, it can lead to diabetes-like symptoms, including high blood sugar levels and insulin resistance. This could explain why some COVID-19 patients develop diabetes during or after their illness.
Future Research and Potential Treatments
While this research provides valuable insights into the effects of SARS-CoV-2 on the pancreas, further studies are needed to fully understand the long-term effects of this interaction. Additionally, understanding this mechanism could lead to new treatments for COVID-19 related diabetes. For example, drugs that block the S1 subunit from binding to ACE2 receptors could potentially prevent or reduce pancreatic damage in COVID-19 patients.
[youtubomatic_search]
FAQ Section
What is the SARS-CoV-2 spike S1 subunit?
The SARS-CoV-2 spike S1 subunit is a part of the virus that allows it to bind to and enter human cells.
How does the S1 subunit cause dysfunction in the pancreas?
The S1 subunit binds to ACE2 receptors in the pancreas, causing inflammation and cell death. This can lead to dysfunction in the pericyte and microvascular of human pancreatic islets.
What are the implications of this dysfunction for COVID-19 patients?
This dysfunction can lead to diabetes-like symptoms in COVID-19 patients, including high blood sugar levels and insulin resistance.
What further research is needed?
Further studies are needed to fully understand the long-term effects of this interaction and to develop potential treatments for COVID-19 related diabetes.
Could this research lead to new treatments for COVID-19 related diabetes?
Yes, understanding this mechanism could potentially lead to new treatments that prevent or reduce pancreatic damage in COVID-19 patients.
Conclusion: The Crucial Role of the SARS-CoV-2 Spike S1 Subunit in Pancreatic Dysfunction
In conclusion, the SARS-CoV-2 spike S1 subunit plays a crucial role in causing dysfunction in the pericyte and microvascular of human pancreatic islets. This dysfunction can lead to diabetes-like symptoms in COVID-19 patients, adding another layer of complexity to this already challenging disease. Further research is needed to fully understand this mechanism and its long-term effects, but these findings could potentially lead to new treatments for COVID-19 related diabetes.
Key Takeaways Revisited
- The SARS-CoV-2 spike S1 subunit can cause dysfunction in the pericyte and microvascular of human pancreatic islets.
- This dysfunction can lead to diabetes-like symptoms in COVID-19 patients.
- The S1 subunit binds to ACE2 receptors in the pancreas, causing inflammation and cell death.
- Further research is needed to understand the long-term effects and develop potential treatments.
- These findings could potentially lead to new treatments for COVID-19 related diabetes.

Leave a Reply