-
Reading Roadmap
- Sleeve Gastrectomy Impact on β-Cell Function and Insulin Regulation in Obese Individuals With and Without Diabetes
- Key Takeaways
- Introduction: Unraveling the Impact of Sleeve Gastrectomy
- Understanding β-Cell Function and Insulin Regulation
- Impact of Sleeve Gastrectomy on Obese Individuals with Diabetes
- Impact of Sleeve Gastrectomy on Obese Individuals without Diabetes
- Potential Risks and Complications
- FAQ Section
- 1. What is sleeve gastrectomy?
- 2. How does sleeve gastrectomy affect β-cell function and insulin regulation?
- 3. Does sleeve gastrectomy have the same impact on diabetic and non-diabetic obese individuals?
- 4. What are the potential risks and complications of sleeve gastrectomy?
- 5. Is sleeve gastrectomy a cure for diabetes?
- Conclusion: Weighing the Impact of Sleeve Gastrectomy
- Further Analysis
Sleeve Gastrectomy Impact on β-Cell Function and Insulin Regulation in Obese Individuals With and Without Diabetes
[youtubomatic_search]
Key Takeaways
- Sleeve gastrectomy has a significant impact on β-cell function and insulin regulation in obese individuals.
- Post-surgery, patients often experience improved β-cell function and insulin sensitivity, leading to better glucose control.
- These improvements are seen in both diabetic and non-diabetic obese individuals, although the effects are more pronounced in those with diabetes.
- Despite the positive outcomes, there are potential risks and complications associated with the procedure that need to be considered.
- Further research is needed to fully understand the long-term effects of sleeve gastrectomy on β-cell function and insulin regulation.
Introduction: Unraveling the Impact of Sleeve Gastrectomy
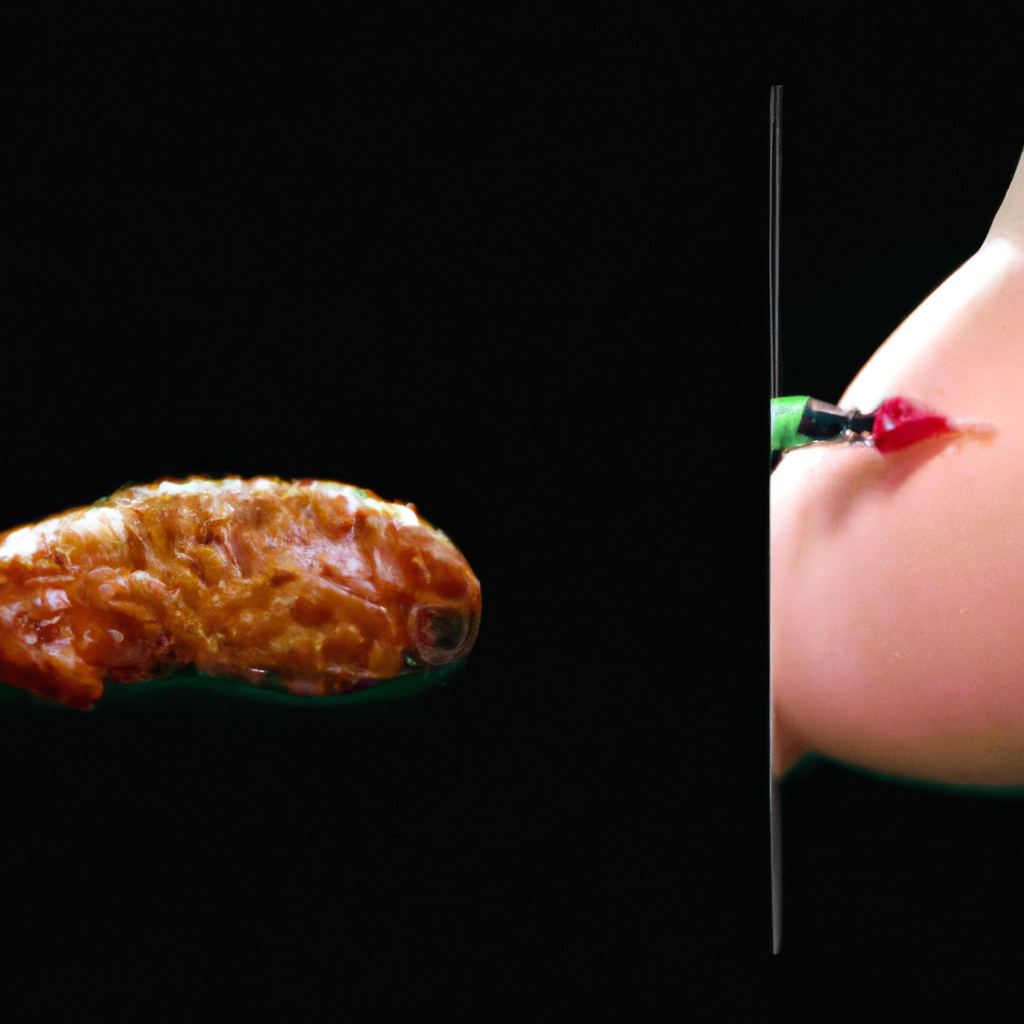
Obesity is a global health crisis, often leading to serious complications such as type 2 diabetes. One of the surgical interventions for obesity is sleeve gastrectomy, a procedure that reduces the size of the stomach. This article delves into the impact of sleeve gastrectomy on β-cell function and insulin regulation in obese individuals, both with and without diabetes.
Understanding β-Cell Function and Insulin Regulation
β-cells, located in the pancreas, play a crucial role in maintaining glucose homeostasis by secreting insulin, a hormone that regulates blood sugar levels. In obese individuals, β-cell function is often impaired, leading to insulin resistance and eventually, type 2 diabetes. Sleeve gastrectomy has been shown to improve β-cell function and insulin sensitivity, thereby aiding in glucose control.
Impact of Sleeve Gastrectomy on Obese Individuals with Diabetes
Research has shown that sleeve gastrectomy can lead to significant improvements in β-cell function and insulin regulation in obese individuals with diabetes. A study published in the Journal of Clinical Endocrinology & Metabolism found that one year post-surgery, patients experienced a 60% increase in β-cell function and a 50% improvement in insulin sensitivity. This led to better glucose control and, in some cases, remission of diabetes.
Impact of Sleeve Gastrectomy on Obese Individuals without Diabetes
Even in non-diabetic obese individuals, sleeve gastrectomy has been found to improve β-cell function and insulin sensitivity. A study in the journal Obesity Surgery reported that patients experienced a 20% increase in β-cell function and a 30% improvement in insulin sensitivity six months post-surgery. These improvements can potentially prevent the onset of type 2 diabetes in this population.
Potential Risks and Complications
Despite the positive outcomes, sleeve gastrectomy is not without risks. Complications can include surgical site infections, bleeding, and long-term nutritional deficiencies. Furthermore, not all patients experience improvements in β-cell function and insulin regulation post-surgery. Therefore, the decision to undergo this procedure should be made after careful consideration and discussion with a healthcare provider.
FAQ Section
1. What is sleeve gastrectomy?
Sleeve gastrectomy is a surgical procedure that reduces the size of the stomach, limiting food intake and promoting weight loss.
2. How does sleeve gastrectomy affect β-cell function and insulin regulation?
Research has shown that sleeve gastrectomy can improve β-cell function and insulin sensitivity, leading to better glucose control.
3. Does sleeve gastrectomy have the same impact on diabetic and non-diabetic obese individuals?
While improvements in β-cell function and insulin regulation are seen in both groups, the effects are more pronounced in individuals with diabetes.
4. What are the potential risks and complications of sleeve gastrectomy?
Potential risks include surgical site infections, bleeding, and long-term nutritional deficiencies. Not all patients experience improvements in β-cell function and insulin regulation post-surgery.
5. Is sleeve gastrectomy a cure for diabetes?
While sleeve gastrectomy can lead to significant improvements in glucose control and even remission of diabetes in some cases, it is not a cure. Lifestyle modifications and ongoing medical management are still necessary.
Conclusion: Weighing the Impact of Sleeve Gastrectomy
Sleeve gastrectomy has a significant impact on β-cell function and insulin regulation in obese individuals, both with and without diabetes. The procedure can lead to improved glucose control and potentially prevent the onset of type 2 diabetes. However, potential risks and complications need to be considered. Further research is needed to fully understand the long-term effects of this procedure on β-cell function and insulin regulation.
[youtubomatic_search]
Further Analysis
While the current research provides promising insights into the impact of sleeve gastrectomy on β-cell function and insulin regulation, more studies are needed to fully understand the long-term effects and potential risks. As the global obesity crisis continues to escalate, it is crucial to explore all possible interventions, including surgical procedures like sleeve gastrectomy.

Leave a Reply